Change is the inevitable truth that nature teaches us! As we age, bodily changes may be very difficult to accept for some, especially if you are not well informed with how your body would change, creating possible pain during menopause. Our bodies go through cycles of change, and oftentimes, change can be both painful and scary. Staying informed and educated about these changes is empowering.
Puberty is openly discussed in school and we seem to be better educated with puberty, however, it is surprising to discover in the clinic, how misinformed women actually are when it comes down to menopause, which in turn leaves women suffering from pelvic pain during menopause.
Very often we start getting intrigued by the word menopause only when our inner clock starts calling its dues. We learn that our fertility starts to slow down, our periods get irregular and very often around the age of 50, the menstrual cycle slows down to its ultimate stop.
However, menopause can occur earlier (as early as 35) for a variety of reasons, some of them could be hormonal, genetic predisposition, surgical, in the form of a hysterectomy and many more. It is important to know about menopause and what to expect so that we can seek medical advice and avail Pelvic PT services at the earliest if need be.
Through menopause, female bodies experience many changes, these changes can be associated with a variety of symptoms, often painful and sometimes puzzling.
Since information about menopause is not shared as commonly, women all over the globe are going through this change unassisted. I strongly feel that this topic needs its due diligence by sharing the knowledge about it and spreading awareness about menopause.
Treating women with pelvic pain is what I specialize in as a pelvic floor PT. So in this blog, I am attempting to discuss the topic of pelvic pain during menopause and what it entails.
Pelvic Pain During Menopause
- Sexual function:
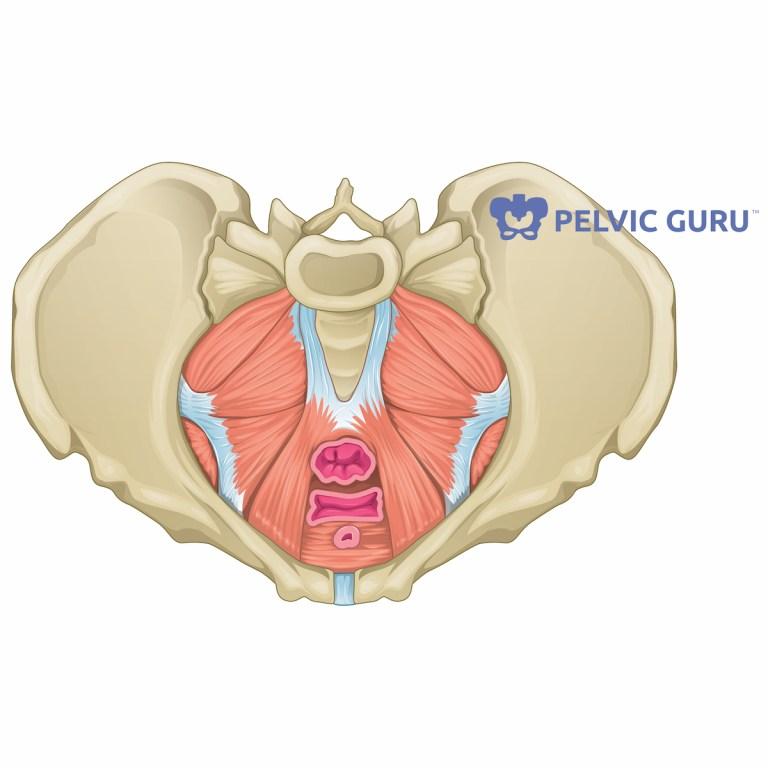
The pelvis and the pelvic floor muscles have varied functions like supporting the visceral organs and severing as the bottom sling support of our visceral cavity along with reproductive ad excretory functions.
Our pelvic floor is responsible for optimizing our sexual response and thus has a key role in preserving our sexual function. During menopause, hormones change and estrogen levels go down. Estrogen helps keep the vaginal tissue happy and healthy, once it starts falling, it makes the tissue drier and thinner making sex painful, which in turn can be detrimental to your overall sexual health, which is why moisturizing lubricants are needed to keep the tissue healthy and sex painless.
As menopause approaches it is important to practice proper vulvar and vaginal care. It is critical to make sure that you are using safe as well as effective techniques for vulvovaginal care.
Here are some tips to maintain a healthy vagina and vulva:
- Try to avoid soap if possible, however, if you feel the need to use it, make sure it’s unscented and very gentle.
- Don’t use washcloths, these can harbor bacteria which can be irritating.
- Use cotton underwear.
- Avoid using tight clothes around the area.
- If you go swimming, make sure to change out of the wet clothes after you are done.
- Hypertonic muscles:
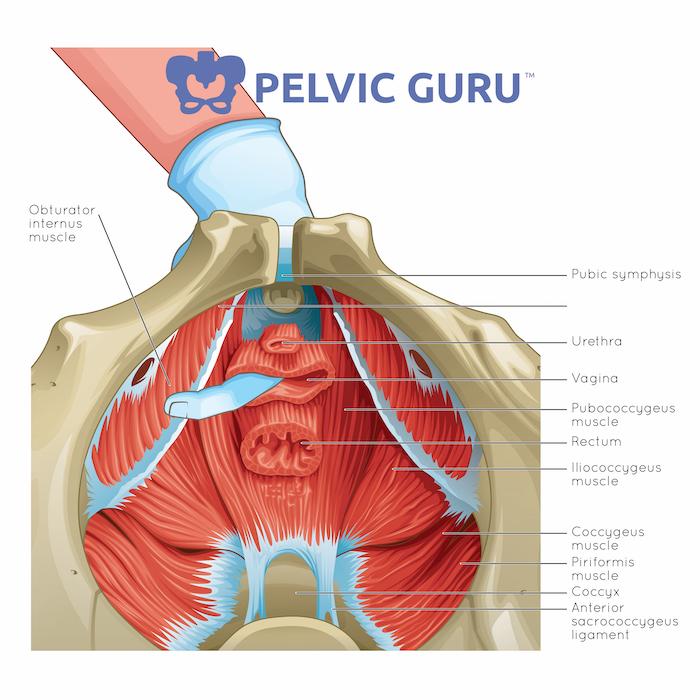
With the onset of menopause as the estrogen levels dip, the pelvic floor muscles often get thinner dryer and tend to develop several trigger points inside the pelvic floor, which may lead to pelvic floor muscle tightness or pelvic pain during menopause. In physical therapy/ pelvic pain jargon, we address it as “overactive pelvic floor muscles”.
I commonly see female patients who, while undergoing menopausal changes, may present with pain during sex even with the use of lubricants. If sexual pain is still present even with the proper use of vaginal lubricants, I recommend a visit to your pelvic pain specialist (OB-GYN specializing in pelvic pain). More than 90% of the time you will also be referred to a pelvic floor physical therapist by your physician.
It is critical that you first get a medical diagnosis for your pain as sexual pain may not always be muscle related. The MD who specializes in pelvic pain with examine your vaginal muscles internally and will be able to accurately determine what is the cause of your pelvic pain. At a Pelvic PT visit, you will be further evaluated to determine the exact group of muscles that need treatment.
In our practice, we believe in thorough evaluation and treatment of pelvic pain by examining the musculoskeletal well being of each and every pelvic floor muscle. We also believe that it is very important to look at the whole person and address other musculoskeletal deficits that may be contributing to pelvic pain.
- Vaginal Atrophy:

The Mayo Clinic describes vaginal atrophy as:
“Vaginal atrophy (atrophic vaginitis) is thinning, drying and inflammation of the vaginal walls that may occur when your body has less estrogen. Vaginal atrophy occurs most often after menopause. For many women, vaginal atrophy not only makes intercourse painful but also leads to distressing urinary symptoms.”
Thinning of vaginal tissue could cause sexual intercourse to be extremely painful. Vaginal muscle atrophy may cause the vaginal canal to narrow, there may also be associated with urinary symptoms such as a burning sensation while urinating, increased urinary urgency increased urinary frequency, and increasing predisposition to UTIs.
It is important to talk to your MD regarding these symptoms as ignorance will only make these symptoms worse. Very commonly, your gynecologist might prescribe a medical treatment ( hormonal- like topical estrogen or nonhormonal – hyaluronic acid-based vaginal lubricants).
However, it is very important to know that pelvic floor physical therapy can also be extremely helpful as we can help you combat the narrowing of your vaginal canal with a vaginal dilator program, as well as help you with the urinary symptoms as we can properly assess and accurately address trigger points in your pelvic floor muscles.
Biofeedback for pelvic floor relaxation or strengthening id a very useful modality of treatment that we often use with pelvic floor physical therapy.
- Urinary Incontinence

One of the very common and concerning symptoms associated with menopause could be urinary incontinence. Urinary incontinence is defined as: “the involuntary leakage of urine. It means a person urinates when they do not want to. Control over the urinary sphincter is either lost or weakened. Urinary incontinence is a common problem that affects many women specifically after menopause.”
As we enter menopause due to dip in estrogen levels and age-associated muscle atrophy, pelvic floor muscles can grow weaker. Pelvic floor physical therapy can be immensely helpful as we can help the pelvic floor muscle get stronger and integrate that into other whole-body exercises, reducing pelvic pain during menopause.
We use specific modalities like Biofeedback therapy and pelvic ultrasounds to train the pelvic floor muscles in a pelvic floor physical therapy clinic. It is important to note that good and healthy vaginal tissue supports a good urethral closure, which will reduce the incontinence and the chances for infection in the area.
- Pelvic organ Prolapse:
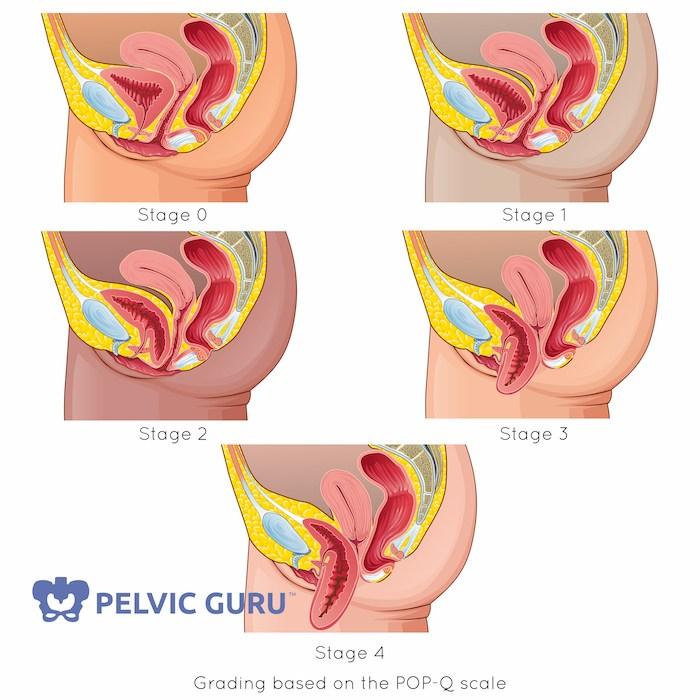
Pelvic organ prolapse is nothing but a downward descent of your pelvic organs and might happen when the muscles and tissues supporting the pelvic organs (the uterus, bladder, or rectum) become weak or loose. This allows one or more of the pelvic organs to drop or press into or out of the vagina. Many women are embarrassed to talk to their doctor about their symptoms or think that their symptoms are normal. But pelvic organ prolapse is treatable.
It is important to remember that the pelvic floor muscles support the pelvic organs like a hammock. It is important to understand that pelvic organs include the bladder, uterus and cervix, vagina, and rectum, which is part of the bowel. A prolapse happens when the pelvic muscles and tissues can no longer support these organs because the muscles and tissues are weak or damaged.
This causes one or more pelvic organs to drop or press into or out of the vagina. Menopause very commonly can lead to symptoms of prolapse as pelvic floor muscles may get weaker secondary to the shift in the hormonal balance.
Pelvic organ prolapse is a type of pelvic floor disorder. The most common pelvic floor disorders are:
- Urinary incontinence (leaking of urine)
- Fecal incontinence (leaking of stool)
- Pelvic organ prolapse (weakening of the muscles and tissues supporting the organs in the pelvis)
Here is a list of potential symptoms you might be experiencing if you have a prolapse:
- As mentioned, a dull heavy feeling in the pelvis.
- Pressure in the pelvis without apparent reason.
- A visible bulge coming out of the vagina.
- Having a difficult time emptying the bladder or bowel.
- Using a splinting maneuver to be able to complete bowel movement.
In conclusion
Menopause is not as easy as magically stopping your menstrual cycle, it’s a whole process and it takes a long time, anywhere from 5 to 10 years as your body adapts again to a new harmony.
If you are experiencing any of the symptoms that we have described for pelvic pain during menopause, please, find your nearest pelvic floor specialist, there’s no need to suffer in silence through menopause, there are ways to help and be helped, making sure this process is easier on your body and your mind.
Feel free to comment and ask me any questions you may have. I’d love to be able to answer them and connect with you. Also, remember to follow me on Instagram for more pelvic floor related content, or check out my blog for older pieces of content you can check!


Recent Comments