The most effective and evidence-based solution for Interstitial Cystitis, or IC, is most definitely Pelvic Floor Physical Therapy, but why is that exactly?
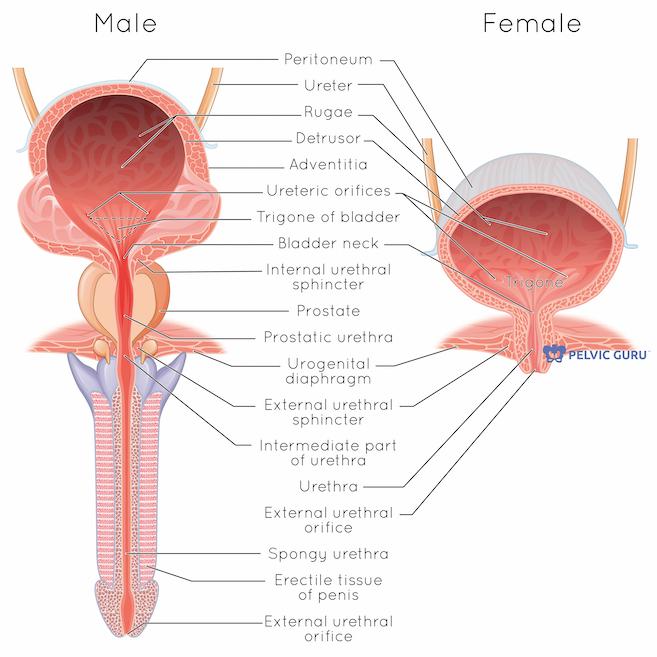
Interstitial Cystitis, or IC, is a chronic and extremely debilitating condition of the urinary bladder. This condition is usually accompanied by excessive urgency and frequency of urination, suprapubic pain, dyspareunia or pain during or after sex, chronic pelvic pain, and negative urine cultures for any potential infections. The symptoms with this condition can vary from person to person, depending on many factors and triggers.
Some of the triggers that can flare up an IC episode can be: menstruation, sitting down for a long period of time, exercise, sexual activity, and others, the signs or symptoms you can experience during a flare-up can be:
- Pain in your pelvis or between the vagina and anus in women
- Pain between the scrotum and anus in men (perineum)
- Chronic pelvic pain
- A persistent, urgent need to urinate
- Frequent urination, often of small amounts, throughout the day and night (up to 60 times a day)
- Pain or discomfort while the bladder fills and relief after urinating.
- Pain during sexual intercourse.
- Symptoms severity is different for everyone, and some people may experience symptom-free periods.
These may sound similar to a UTI, however, the main difference is the lack of infection when it comes to IC. However, if there is a UTI present in someone already suffering from IC, it will most definitely make the symptoms worse.
IC can make it challenging for the patient to participate in daily and recreational activities without pain or discomfort. Patients often report they have been experiencing a reduced bladder capacity “ I feel like I have a small bladder” and increase urgency which could make trips to the bathroom very frequent. As a result, patients often experience a lower quality of life, as they are constantly being affected by the symptoms associated with IC. Very often, sexual pain is also linked to IC. Pain could significantly affect pain-free sexual intimacy, as well as your mental health. In addition, chronic pain associated with IC can cause a lack of sleep and emotional stress and often lead to a negative spiral of depression.
Pelvic floor PT for Interstitial Cystitis, really?

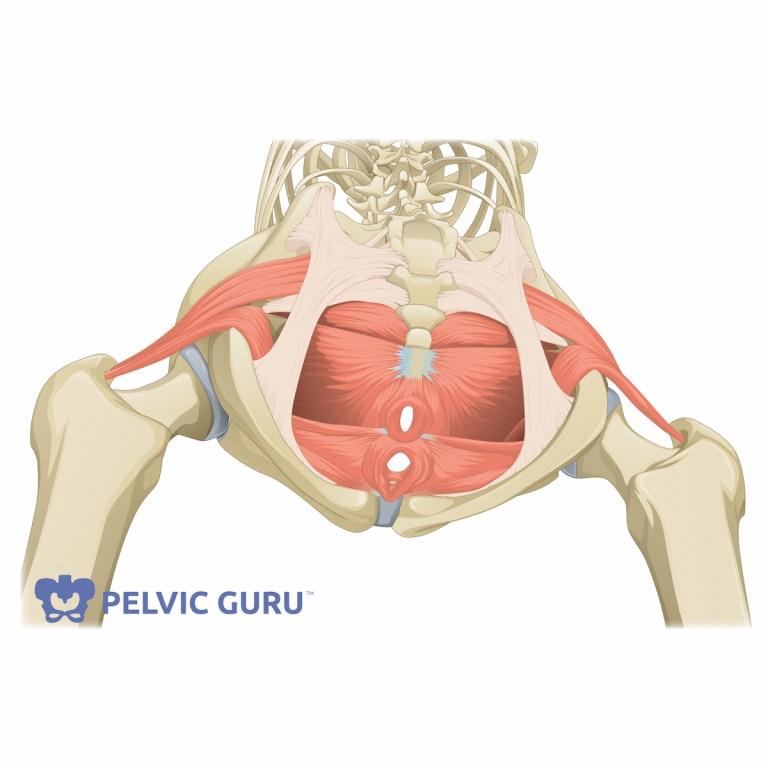
Yes, really! There is a big body of evidence that suggests that in over 85% of patients diagnosed with IC there exists pelvic floor dysfunction! While pain associated with IC can be extremely debilitating, it is important to know that your symptoms may not be entirely linked to the bladder. These symptoms may be occurring because of pelvic floor muscle tightness and the inability of the pelvic floor to relax when needed. There could also be secondary symptoms such as constipation, sexual pain, low back pain, and hip pain,
When treating IC, the first and very important approach that I often use is to suggest simple yet effective changes in your lifestyle. Although by training I am a doctor of Physical Therapy, I make sure my patients understand the importance of dietary changes and an overall view of the behaviors that might be triggering the flare-ups. When appropriate I often refer patients to holistic nutritionists and psychologists. I firmly believe in a team approach when it comes to recovery from complex conditions like IC.
While recovering from IC pelvic floor physical therapy is the backbone of treatment. When treating a patient diagnosed with IC I believe in a multifaceted approach. Once we take a look at the entire set of symptoms, we are more capable of making an effective treatment consisting of a whole-body approach, giving our patients a better chance at having a regular daily routine with limited to no pain.
A recent study very well summarises the importance of pelvic floor PT for Interstitial Cystitis as a recovery method. “A significantly higher proportion of women with interstitial cystitis/painful bladder syndrome responded to treatment with myofascial physical therapy than to global therapeutic massage”, which speaks volumes of the effectiveness of the treatment for this particular condition.
An interesting finding of another study was that patients who went in for the first time for a pelvic floor physical therapy appointment after being diagnosed with interstitial cystitis came in with an average pain level of 7.6 / 10 on that initial evaluation, however, after 6-8 weeks of targeted treatment the pain went down to an average of 2.6/10 when measured on VAS.
Patients have reported over 60% improvement in their pain, the symptoms they were experiencing and how much these limited their daily life. It is important to note that over 54% of patients saw significant improvements in their symptoms within their first 3 PT appointments, 31% saw the improvement during their 4-6 PT appointments. Also, only 15% needed over 6 appointments to see positive results.
These numbers are really motivating for me as a physical therapist, and for my patients, as they can come into an appointment riddled with fear of the unknown. However, it is important to note that there are still so many misconceptions about IC. I would like to take this opportunity to clear some of them up before closing in this blog post.
Misconceptions about IC

The number one misconception I have seen all over is that Interstitial cystitis affects only women and this could not be further from the truth. According to a study published, women comprise 90% of patients with IC however it is important to note that the remaining 10% is all men. It is more common in women, yes, so common in fact that around 700,000 women are affected by this condition in the US alone.
Second misconception, there’s only one kind of IC. No, not true, there are different variations of this condition. Interestingly, the more common kind of IC is non-ulcerative interstitial cystitis, and it happens to 90% of diagnosed patients, while the remaining 10% is of the more severe type, which involves Hunner’s ulcers, which are lesions in the bladder. These often can show up as brown spots on the bladder’s mucosa ( inner lining), making it incredibly painful.
Third misconception, it only happens in adults! No, this condition has been also found in children. Some of the symptoms you can find in children with IC include urinary frequency, sensory urgency, and lower abdominal pain. It is indeed more common to see this condition present itself in middle age women, anywhere from 30 years old to 70 years old.
Something that genuinely shocked me the first time I worked with a patient suffering from IC, is how difficult it was for them to be referred to me, and as time went on I realized they were coming in after searching it up on their own, taking matters into their own hands. Sure enough, it was not a surprise to me when I read that in this particular study, over half of the patients evaluated reported having seen 5 or more medical doctors for their condition and spent around 4 years prior to being formally diagnosed and before they began pelvic floor physical therapy.

This condition is debilitating, but I am happy to report to all of you suffering from it, there is help available, and if you advocate for yourself you’ll be able to get help sooner!!
Do you want to know more about physical therapy in other conditions? I have a blog post talking all about physical therapy and endometriosis.
If you are concerned about your very first PT appointment, fear no more, I have a blog post detailing how it should go!
Follow me on Instagram for more daily content!
References
Fitzgerald, M., Payne, C., Lukacz, E., Yang, C., Peters, K., Chai, T., … Nyberg, L. (2012). Randomized Multicenter Clinical Trial of Myofascial Physical Therapy in Women With Interstitial Cystitis/Painful Bladder Syndrome and Pelvic Floor Tenderness. Journal of Urology, 187(6), 2113–2118. doi: 10.1016/j.juro.2012.01.123
METTS, J. U. L. I. U. S. F. (2001). Interstitial Cystitis: Urgency and Frequency Syndrome. Am Fam Physician, 64(7), 1199–1207. Retrieved from https://www.aafp.org/afp/2001/1001/p1199.html
What is Interstitial Cystitis(IC)/Bladder Pain Syndrome? (n.d.). Retrieved March 11, 2020, from https://www.urologyhealth.org/urologic-conditions/interstitial-cystitis
Prince, S. (n.d.). Pelvic Floor Level 1 – Virginia Beach, VA – March 13-15, 2020 (SOLD OUT). Retrieved March 11, 2020, from https://hermanwallace.com/continuing-education-courses/pelvic-floor-level-1/virginia-beach-va-march-13-15-2020
Interstitial cystitis. (2019, September 14). Retrieved March 14, 2020, from https://www.mayoclinic.org/diseases-conditions/interstitial-cystitis/symptoms-causes/syc-20354357

Recent Comments