Interstitial Cystitis (IC), a relentless affliction impacting over 12 million Americans, beckons exploration into its intricate web of causes, symptoms, treatments, and the pivotal role of pelvic floor physical therapy. As a devoted pelvic floor physical therapist, I endeavor to shed light on this complex journey.
Understanding Interstitial Cystitis:
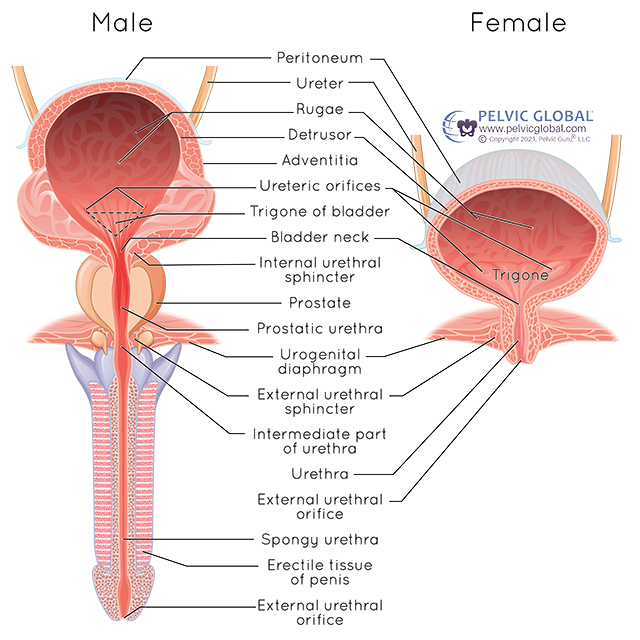
IC, alias painful bladder syndrome, manifests as a relentless interplay of chronic pelvic pain and discomfort, eluding swift diagnosis due to its multifaceted nature. While etiological factors remain elusive, factors like a defective bladder lining, autoimmune reactions, and genetic predisposition contribute. Symptoms encompass chronic pelvic pain, urinary urgency, frequency, painful intercourse, and a sense of incomplete bladder emptying.
Statistics Spotlight:
– Over 12 million Americans are affected by IC.
– Up to 85% of IC patients experience pelvic floor dysfunction.
– Many IC patients report severe pain, surpassing that associated with bladder cancer.
Treatment Options:
Though IC lacks a cure, various strategies strive to alleviate symptoms:
1. Dietary Modifications: Foods and beverages, such as caffeine, alcohol, and spicy items, may exacerbate symptoms.
2. Medications: Prescribed pain relievers, bladder coatings, and muscle relaxants are common treatments.
3. Bladder Instillations: Medications directly instilled into the bladder aim to reduce inflammation.
4. Physical Therapy: Pelvic floor physical therapy stands out as the most proven treatment, recommended by the American Urological Association.
The Role of Pelvic Floor Physical Therapy:
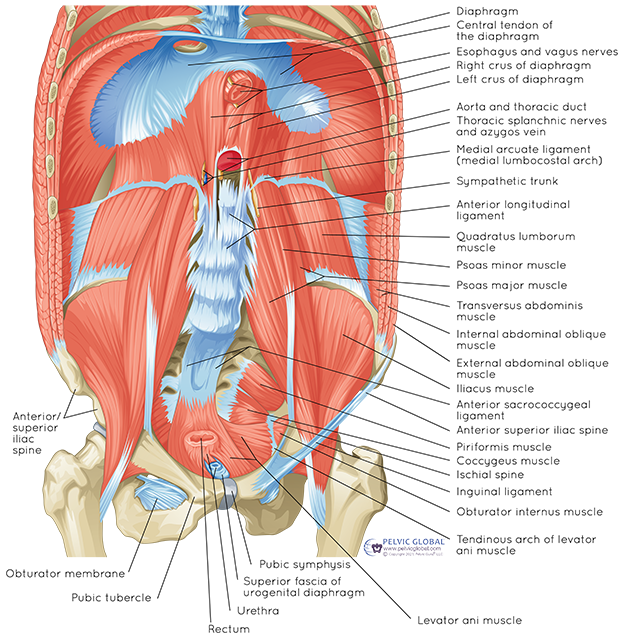
Pelvic floor physical therapy is a specialized branch of physical therapy that focuses on the muscles, ligaments, and connective tissues in the pelvic region. For individuals with interstitial cystitis (IC), pelvic floor physical therapy plays a crucial role in addressing the musculoskeletal and neuromuscular components of the condition. Here are some specific physical therapy treatments commonly employed for individuals with IC:
1. Muscle Relaxation Techniques:
– Stretching Exercises: Targeted stretches help release tension in the pelvic floor muscles, promoting flexibility and reducing muscle tightness.
– Relaxation Techniques: Therapists guide individuals through relaxation exercises to alleviate muscle spasms and promote a more comfortable pelvic environment.
2. Biofeedback:
– Surface Electromyography (sEMG): This technology measures and provides visual or auditory feedback about pelvic muscle activity. Biofeedback helps individuals become more aware of their pelvic floor muscles and learn to control and relax them effectively.
3. Manual Therapy:
– Soft Tissue Massage: Therapists use hands-on techniques to release tension and trigger points in the pelvic floor muscles, enhancing blood flow and promoting healing.
– Joint Mobilization: Manual therapy techniques address joint dysfunction in the pelvic region, improving mobility and reducing pain associated with IC.
4. Pelvic Floor Exercises:
– Kegel Exercises: Controlled contraction and relaxation of the pelvic floor muscles help improve muscle strength and coordination.
– Reverse Kegels: These exercises focus on relaxing and lengthening the pelvic floor muscles, counteracting excessive muscle tension.
5. Behavioral Strategies:
– Bladder Training: Therapists work with individuals to develop strategies for controlling urinary urgency and frequency through timed voiding and gradual increases in intervals between bathroom visits.
– Posture and Body Mechanics Education: Proper body mechanics and posture can significantly impact pelvic floor health. Therapists provide guidance on maintaining optimal alignment to reduce stress on the pelvic region.
6. Functional Training:
– Functional Movement Exercises: Incorporating movements that mimic daily activities helps individuals apply proper pelvic floor muscle engagement in real-life situations.
– Core Strengthening: Strengthening the core muscles helps provide additional support to the pelvic floor, reducing strain and promoting overall stability.
7. Patient Education:
– Lifestyle Modifications: Therapists educate individuals about lifestyle factors that may exacerbate IC symptoms, such as dietary choices, fluid intake, and stress management.
– Self-Care Techniques: Individuals learn self-care strategies, such as proper toileting habits and relaxation techniques, to manage and alleviate symptoms on a daily basis.
8. Collaborative Care:
– Communication with Healthcare Team: Pelvic floor physical therapists often work closely with other healthcare providers, including urologists, gynecologists, and pain management specialists, to ensure a comprehensive and coordinated approach to IC management.
Statistics Spotlight:
– Research indicates that at least 85% of IC patients also have pelvic floor dysfunction.
– Over half (54%) of patients in a study reported an improvement in symptoms within the first three visits of pelvic floor physical therapy.
Pelvic PT’s Transformative Impact:
In a groundbreaking study presented at the International Pelvic Pain Society meeting, thirteen consecutive IC patients shared their transformative journey:
– A staggering 60% improvement in pain, symptom bother, and daily activity limitations.
– Rapid relief observed, with 54% experiencing improvements within the first three visits.
– Initial pain levels, averaging 7.6 out of 10, plummeted to 2.6 after pelvic floor physical therapy.
Statistics Spotlight:
– More than 12 million women and men suffer from IC in the United States alone.
– Shockingly, only 7.7% of respondents believed they were timely referred to pelvic PT by their doctor.
– Nearly half (46%) had to discover pelvic floor physical therapy for IC independently.
The Pelvic Floor and IC: Educating Doctors:
At the conclusion of the first appointment with a new IC patient, a recurring question echoes:
“Why didn’t my doctor tell me about physical therapy for IC years ago?”
In a revealing study, only 14% felt they were referred to PT at the right time, with 43% having to find PT independently and another 43% referred too late as a ‘last resort.’ Shockingly, the American Urological Association recommends physical therapy for IC in the first line of medical treatments.
“Only a fraction of patients with the key symptoms of IC/BPS – urinary frequency, urgency, and pelvic pain – have ulcers within the bladder… we must be willing to look beyond the bladder and examine for pelvic floor issues.” – Dr. Kenneth Peters
Dr. Peters emphasizes the importance of looking beyond the bladder, distinguishing between Hunner’s lesion IC and unexplained pelvic pain. Despite research favoring holistic approaches, many clinicians opt for invasive bladder-focused treatments.
*”We’ve found that identifying and treating pelvic floor dysfunction with modalities such as pelvic floor physical therapy… can frequently resolve or significantly lessen the patient’s pain and bladder symptoms.”* – Dr. Kenneth Peters
Clinical trials affirm the efficacy of pelvic floor physical therapy, offering sustained relief. However, holistic treatment plans, combining physical therapy with other tools, prove most effective.
Interstitial Cystitis is a complex and challenging condition, but with the right approach, individuals can find relief and improve their quality of life. As a pelvic floor physical therapist, I am committed to helping those with IC navigate their journey towards better pelvic health, providing support, education, and personalized treatment plans to address the unique needs of each individual. If you or someone you know is struggling with IC, don’t hesitate to explore the potential benefits of pelvic floor physical therapy, you can schedule your appointment with me, we are still receiving patients in our Armonk PT location!


Recent Comments